
For the fourth edition of ‘TIC Spotlight’ we are focusing on a condition that is “real pain in the butt” quite literally and is often overlooked and ‘misdiagnosed’ as common sciatica. Read on to understand how you can recognise the symptoms of piriformis syndrome and be equipped with the right tools to prevent symptoms from developing further and keep yourself active!
Piriformis Syndrome
What is it?
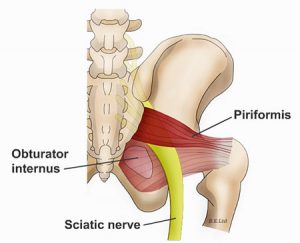
Piriformis syndrome is a condition in which the piriformis muscle, located in the buttock region, becomes overly tight, inflamed or irritated causing pain into the buttock and often back of the thigh. The piriformis muscle itself plays a role in assisting certain movements of the hip helping to rotate the leg and the foot outwards.
Because of its location just under the gluteus Maximus muscle and running diagonally to the sciatic nerve (in around 20% of people the nerve can run through the muscle) when it become tight or inflamed, the piriformis muscle can irritate the nearby sciatic nerve and cause pain, numbness and tingling along the back of the leg and into the foot leading to it often being overlooked and misdiagnosed as sciatica.
Continue reading to understand how you can identify the symptoms of piriformis syndrome and how this is not just your common ‘sciatica’!
Symptoms
Piriformis syndrome is characterised by dull aching pain that originates in the buttock region, and later can radiate into the lower back, the back of the leg and the outside of the foot.
Those with piriformis syndrome will also report persistent dull aching pain that is difficult to relieve and increases when walking up stairs or an incline. Due to the nature of the pain, patients often report symptoms also becoming worse after prolonged periods of sitting and functional activities such as walking, squatting and running. Symptoms can often feel better after lying down flat on the back.
Causes
Primary piriformis syndrome is the cause of anatomical factors relating to the position of the sciatic nerve and the piriformis muscle. However, this is rare and only accounts for around 15% of diagnosed cases.
The exact cause of piriformis syndrome are not fully understood; however likely secondary causes of piriformis syndrome are thought to be due to a sudden stress or trauma to the piriformis muscle.
Other more mechanical causes of piriformis syndrome can be the result of repetitive stress to the piriformis muscle from activities such as distance-walking, running or long periods of sitting on hard surfaces. another factor thought to lead to piriformis syndrome are altered biomechanics in the lower back, pelvic and lower leg regions leading to the muscle becoming short and over-tight.
Any one or a combination of these dysfunctions can lead to compression or irritation of the nearby sciatic nerve.
Females are also six times more likely to experience piriformis syndrome than males due to naturally having a wider pelvic structure.
Common Myths
Piriformis syndrome is just sciatica – False!
Sciatica is not a diagnosis, but rather a symptom of an underlying condition. Sciatica symptoms can be caused by a number of different conditions and it is important to get an accurate diagnosis for the cause of sciatica symptoms.
You can’t exercise if you have piriformis syndrome – False!
Whilst activities that aggravate symptoms will need to be modified, a contributing factor to piriformis syndrome is weak gluteal muscles causing an overload of the piriformis muscle, so it is imperative to strengthen them! Gentle movement around the back and hip can also help ease symptoms.
How is it treated?
A number of conservative treatment methods are commonly used to reduce pain and restore normal function in those suffering with piriformis syndrome. These include:
- Therapeutic ultrasound
- Soft tissue techniques including sports massage or medical acupuncture
- Piriformis muscle stretching
- Hot and cold treatments
- Lower back treatments
- Home exercise programmes aimed at strengthening weak muscles around the hip and restoring faulty movement patterns.
In more severe cases an ultra-sound guided injection may be considered to reduce inflammation of the piriformis muscle if conservative methods have failed to reduce the pain.
Surgery is only considered in a small number of cases when non-surgical management has failed and symptoms have become disabling.
What Can You Do?

It’s important to avoid long periods of sitting and aim to stand or walk every 20 minutes – this will reduce compression to the piriformis and sciatic nerve.
Stretch the piriformis and gluteal muscles, along with the lower back daily to reduce tension around the lower back and pelvic regions.
Simple Piriformis stretch: Lie on your back with your legs straight on the floor. Bend the knee of your affected side and bring it up towards your opposite shoulder. You should feel a comfortable stretch, not pain, in your buttock muscles.
Apply ice to the buttock area regularly to reduce inflammation in the muscle and help to ease pain.
If you’ve found the information in this article interesting and are wondering what else we can help you with? Then please feel free to get in touch with us here at the clinic.
